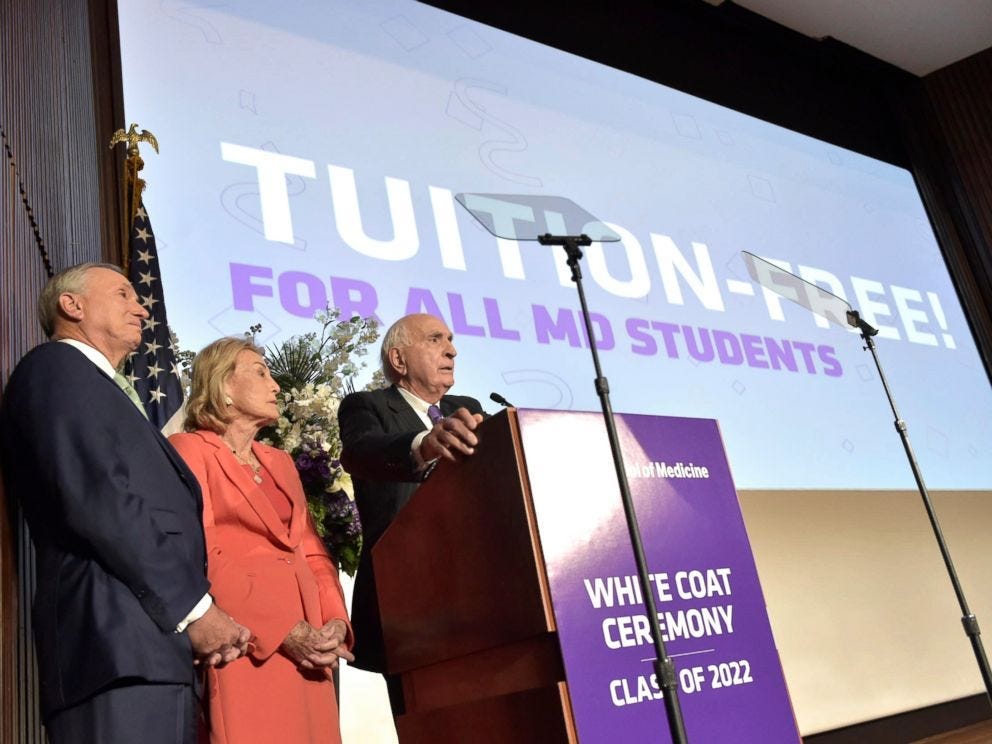
Johns Hopkins is the latest med school to become tuition-free, thanks to a $1 billion donation from Billionaire Michael Bloomberg. The gift applies to anyone whose family earns less than $300,000 annually. Instead of writing about this issue anew, I am “restacking” a piece I wrote when NYU went tuition-free years ago, during my medical school days. The TLDR is this is unlikely to solve our society’s primary care shortage problem. It’s a huge gift to people with some of the highest earning potential in our society and not an effective allocation of resources. More below.
“Why didn’t I apply to NYU?” is the first thought that went through my mind when New York University School of Medicine announced last week that it will make medical school tuition-free for all incoming and returning students. I was excited for my peers 2 hours south on Interstate 95. Addressing the debt burden for medical trainees is important, as medical school has become increasingly expensive over the last decades. After giving it further thought, I think the funds could be allocated more thoughtfully given the medical school’s intent: to increase the number of students going into primary care and increase socioeconomic diversity among the medical school’s student body.
“NYU also says medical school debt is ‘reshaping the medical profession,’ as graduates choose more lucrative specialized fields in medicine than primary care […] The school hopes the plan will also increase diversity among its students — what it calls ‘a full retrofitting of the pipeline that trains and finances’ future doctors.” James Doubek, NPR.
America is facing a looming shortage of primary care physicians: the estimated shortage will be between 8,700 and 43,100 physicians nationally by 2030, according to a recent report by the AAMC. Reports attribute medical students’ gravitating towards specialties to higher pay. Specialists earn an average of $316,000, while primary care physicians earn an average of $217,000. Reports would say that this near-additional $100,000 yearly is preferred because of the debt students incur while in medical school. However, a recent report published in JAMA suggests that debt is likely less determinant of specialty choice than future income. We do, of course, function in a healthcare system that undervalues primary care. This has been palpable at my medical school. Research is highly prioritized, and specialties are emphasized early on. There is a dearth of mentors for students interested in primary care. At the time of residency applications, students interested in family medicine must be advised by a faculty person based out of a neighboring medical school… because we do not have a family medicine department. Neither does NYU.
Medical schools that prioritize training primary care physicians for the communities in which they are located make it clear at every stage of their medical education process. They state it in their mission statements and emphasize it during the four years of training. Morehouse School of Medicine, for example, was created to increase the number of primary care physicians in Georgia. Morehouse placed first in the medical school social mission ranking, a tool used to measure and compare schools’ social impact based on the number of graduates who practice primary care, work in health professional shortage areas, and are underrepresented minorities. NYU, conversely, landed the 5th lowest in the same ranking. These schools attract and select different types of students, largely because of their mission vis-à-vis society. Prestigious schools will likely select students who perform well on standardized tests and have robust research experience. In contrast, more socially oriented schools select students who may also grapple with inequality besides meeting the qualifications for admission. That is not to say that all students who perform well on standardized tests do not grapple with inequality, but facing inequalities certainly impacts students’ ability to do so.
I’d argue that the financial incentive for students interested in primary care should be disbursed through a loan forgiveness program, requiring that the beneficiaries commit a certain number of years to practice primary care, akin to the National Health Service Corps loan repayment program. A similar model has been adopted by several institutions of higher learning, where graduates who go into public interest or non-profit work instead of high-paying jobs receive a sliding-scale rebate on their business or law school loans.
Furthermore, most medical students come from the top two family income quintiles. This majority can afford the resources required to prepare for and eventually get into medical schools. Making medical school tuition-free for all to help students from a lower socioeconomic status should go hand in hand with committing to breaking down barriers that keep those students from entering medical schools. All other things being equal, this policy would otherwise make NYU more attractive to the same pool of applicants who face the tough choice of picking which prestigious medical school to attend. When asked in a previous interview about financial aid initiatives aimed at students from marginalized backgrounds, Yale School of Medicine’s dean, Dr. Robert Alpern, said:
“We all offer scholarships to steal students from other schools, to save our own skin, but in fact we don’t do anything for the country. All we do is shuffle these students around. A more comprehensive solution would be beyond the university’s capacity.”
Having raised nearly half a billion dollars, NYU has a certain capacity to contribute to more comprehensive efforts. It may be more socially impactful to broaden the pool of applicants by taking into even greater consideration factors outside of test scores and elements tied to privilege and by making significant financial contributions to sustainable pipeline efforts and additional support for current underprivileged medical trainees. As mentioned, Morehouse is a leader in this realm, having invested in 9 K-12, six undergraduate, and two post-baccalaureate pipeline programs.
To be sure, the debt burden for the average medical graduate is exorbitant, and medical schools, along with policymakers, should put forth efforts to make medical education more accessible and affordable, compromising perhaps on need-based policies. Take a completely different system, France: like the rest of higher education, medical school is free for all, and the government carries the cost burden. In exchange, the government works with physician unions to ensure that the cost of healthcare remains affordable, which in part makes medicine less lucrative than it is in the U.S. Additionally, the income gap between specialists and general practitioners is noticeably smaller: in 2016 the median income for generalists/primary care providers was 79,600€, and for specialists, it was 80,000€: a gap of less than $1000, about 100 times less than the current gap in America. For those who understandably blame shying away from primary care on the debt burden, the question is whether they would be truly satisfied with the salary primary care physicians currently earn in exchange for tuition-free medical school.
Before other medical schools with colossal endowments or fundraising capacity race to make attendance tuition-free for all, I would caution the leaders to study the impact it would have on our society carefully. It is a powerful statement to be able to support so many students’ education. Still, it would be even more powerful to use those funds with more intentionality when targeting the shortage of primary care providers and aiming to address diversity issues in medicine.